Weaknesses and corruption in the health system of Bangladesh came in the spotlight in 2020 as the country endured the first-ever outbreak of the deadly COVID-19 that defined the year globally.
The viral disease, that gradually engulfed the world, was at the centre of attention throughout the year, exposing the country’s poor preparedness for such a health crisis, along with instances of mismanagement and deep-rooted corruption coming out one after another.
Still the challenges persist centering COVID-19 that has so far infected over 5.10 lakh people and killed nearly 7,500 in the country, while experts said that lack of preparations for fighting the menace and of monitoring and accountability in procuring medical supplies have not been addressed effectively.
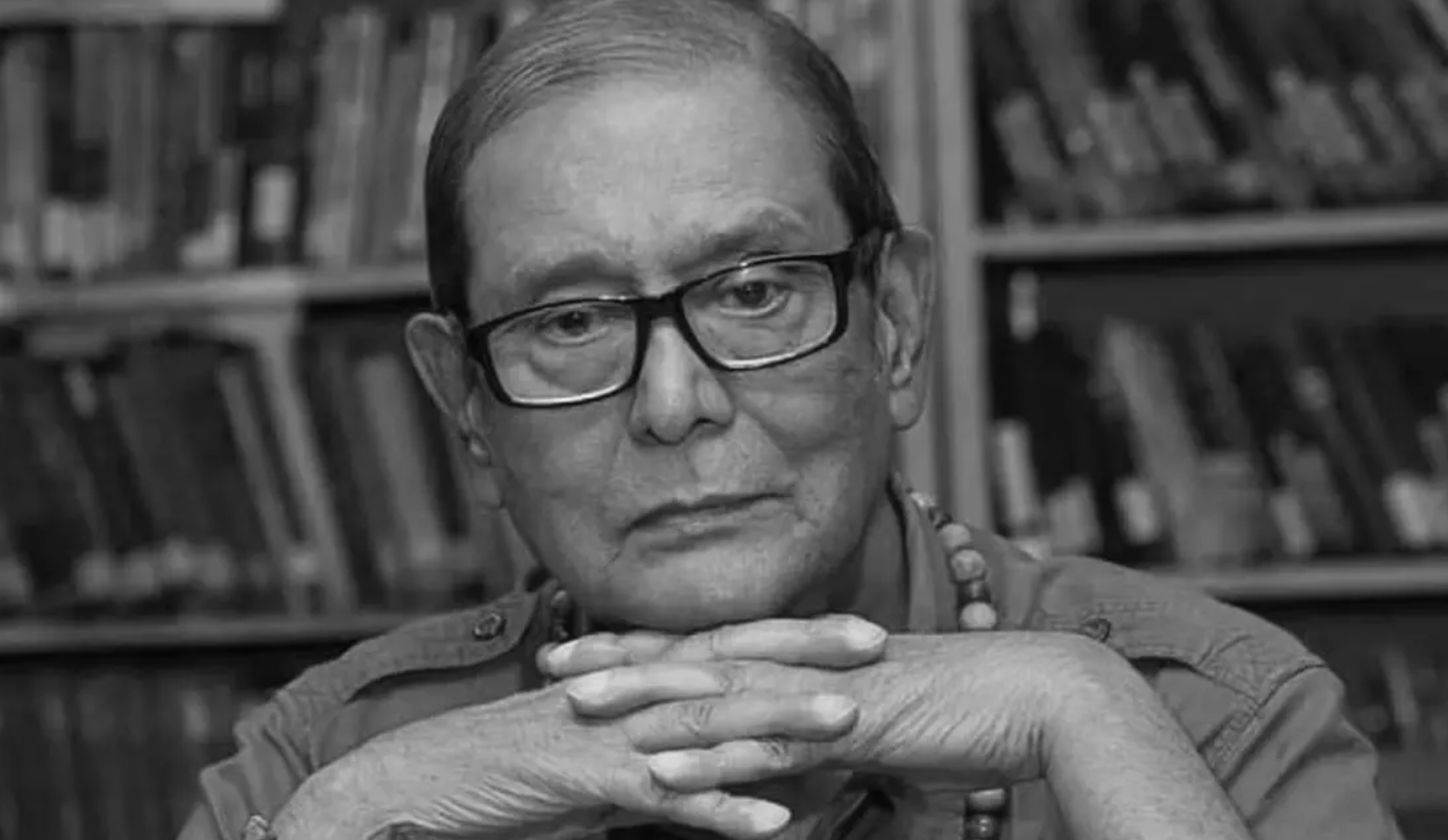
‘What people really received in terms of health care in 2020 remains a big question, but corruption for money making by a quarter in the health sector did not relent despite the emergence of an unprecedented humanitarian crisis due to COVID-19,’ said noted public health expert and freedom fighter Zafrullah Chowdhury.
‘This year could be termed as a year of anarchy for the health sector: the government did not take effective measures to prepare the country’s health system for the crisis but indulged in corruption and people did not obtain expected services while doctors evaded their duties,’ said Zafrullah, also founder of Gonoshasthaya Kendra.
A global alarm over the novel coronavirus was raised in late December of 2019 after it originated in China, but Bangladesh, though being closely connected with the country, and its neighboring countries acted late to close their borders and ensure proper screening at international arrival points.
On March 8, 2020, Bangladesh confirmed its first three COVID-19 cases, but the virus had already entered the country in February from various international sources, spreading all over the country by March, as revealed by an Institute of Epidemiology, Disease Control and Research study.
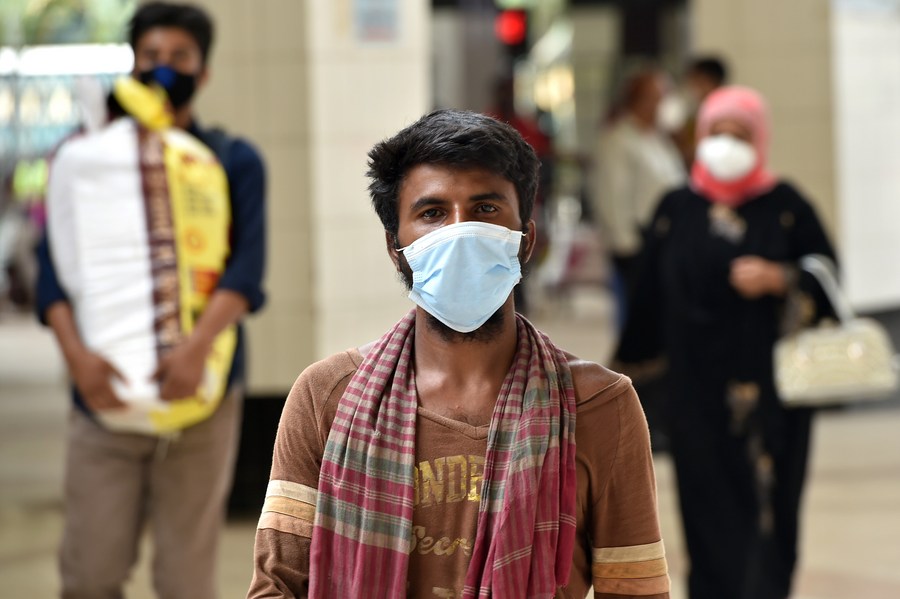
Testing, isolating and quarantining suspected cases were in jeopardy while the IEDCR, the disease monitoring arm of the government, relied only on the one testing lab in the capital with no institutional quarantine facilities put in place.
Incidents of hospitals turning down suspected patients, doctors and other healthcare providers bypassing their duties and their neglect to hospitalised patients abounded while the number of patients increased across the country.
Patients with COVID-19 symptoms were hard put to access healthcare services, get tests done, and secure isolation beds while contact-tracing, an important measure to arrest the infection, was first non-existent and later marred by mismanagement.
While hospitalised patients did not receive quality care at the COVID-19 dedicated hospitals, there were many others who failed to obtain care, fast raising the national death tally.
The situation shattered the confidence of people in the country’s health system, prompting them to turn away from the hospitals, especially for COVID-19 care.
COVID-19 patients died at home after deciding not to go to hospitals.
Since mid-May, at least 735 COVID-19 patients across the country have died outside hospitals — 701 at home and 34 on the way to hospitals, according to the Directorate General of Health Services.
‘People lost their confidence in the healthcare services that led them to opt for staying at home even when they are dying,’ said public health expert Rashid-e-Mahbub.
‘The experience of the denial of treatment when badly needed and the absence of quality care after hospitalisation shattered the trust of people [in the health system],’ he observed.
The government initially struggled to address the inability to conduct tests and develop infrastructures for patients, but when it and donors allocated funds for the preparation and procurement of medical supplies big scams and shady deals undermined the process.
Regent Hospital in the capital hogged headlines after the Rapid Action Battalion exposed its irregularities, including the business of issuing fake COVID-19 certificates, and undue privileges enjoyed by its owner because of his political clout.
Hard on the heels of fake N95 masks supply by a company favoured by government officials and Regent’s test scam, more such scams surfaced.
JKG Health Care authorities were also caught red-handed in the act of issuing fake coronavirus test reports, affecting hundreds of migrant workers’ travel to their destination countries as the western media reported that Bangladeshi migrants carried fake COVID-19-free certificates while travelling.
The involvement of officials of the Directorate General of Health Services in the scams led to major changes in the national health agency, including the removal of its director general, but health m